Partial (Unicompartmental) Knee Replacement
Author: Dimitrios Giotikas MD, PhD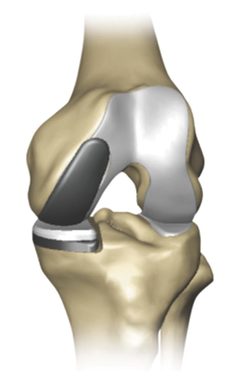
Partial or Unicompartmental (or UNI) knee replacement is a procedure which involves the replacement of the medial half of the knee only.
Obviously it is indicated for less severe cases of knee osteoarthritis contained only to the medial half of the knee. These patients can still get a lot of pain during their activities , not responding well to medications and other nonoperative treatments. Often they belong to a bit younger age group than their counterparts with total knee replacement (TKR), although UNI is indicated for any age group with contained osteoarthritic change.
Its main advantage compared to the TKR is that it provides a slightly better functional outcome and a more natural feeling in the knee. Most importantly, it preserves more bone stock for future re-operations (conversion to TKR) compared to a TKR. This younger, and more active age group will probably exceed the lifespan of their prosthesis (either UNI or TKR) and will require a revision or conversion) anyway.
The survivorship of the UNI systems is comparable to TKR systems and is reported to be 94% in 15 yers.
The results of conversion to TKR after UNI are comparable to the results of revision TKR after Primary TKR, and after primary TKR in not previously operated knees. The operation is done under general or regional spinal anaesthesia. This is anaesthtist’s decision but if you have any preference they are happy to follow it if there aren’t any contraindications. The patient is positioned supine on the operating table. A minimally invasive (MIS) approach of approximatelly 12-14 cm length is placed just on the medial side of the patella (Kneecup).
It is worth saying that it was the good results of the MIS approach to UNI in the first place which introduced the concept of MIS approaches to the field of knee replacement. The surgeon then inspects the condition of all the compartments of the knee and confirms that a UNI is indicated. Sometimes despite the appearances on the xray or the MRI before the surgery, the lesions are more extensive on direct visual inspection than shown preoperatively.
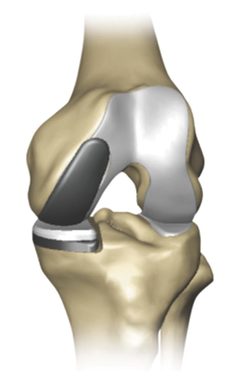
In this case a total knee replacement may be more appropriate for the patient. All candidates for UNI are informed about this possibility. The surgeon then removes with the use of special guides and instruments the surfaces of the medial halves of femur and tibia and replaces them with the prosthesis system. The prostheses system includes a femoral component a tibial component and an insert between them. Implant systems in joint replacements are generally judged based on their functional ourcomes, the occurence of any implant related complication and their survivorship.
UK NJR (National Joint Registry) and
ODEP (Orthopaedic Data Evaluation Panel) ratings provide useful data about the implants’ performance.
The important part of the technique is to replace the removed bone with implants of equal total thickness in order to restore proper soft tissue tension. The surgeon has specific ways of assessing the soft tissue tension during the procedureBlood loss is not expected to be much because a tight cuff (tourniquet) is placed on the thigh to stop the blood from running into the surgical field. We also use transexamic acid, a medication which is indicated for reducing the bleeding from the surgical field. The use of local infiltration with analgesic and epinephrine reduces further the bleeding.The wound is closed meticulously in layers and the skin is sutured with cosmetic subcuticular (under the skin) suturing technique and absorbable stitch which doesn’t need to be removed.
At Giotikas Orthopaedics we follow the
UK GMC (General Medical Council) Guidelines on discussing the risks and complications of any proposed intervention. All related risks are explained and discussed thoroughly on an individualized bases during the preoperative consultation of the patient.
Risks related with UNI knee replacement include:
• Infection
After surgery an infection may occur in the skin over the wound or deep in the wound. An infection may happen while you are in the hospital or after you go home. You will be given antibiotics before the start of your surgery and these will be continued for about 24 hours afterward to prevent infection.
Deep infection happens in around 1% of the cases. It is rather rare but when it happens it usually requires further surgeries and long term antibiotics for 6 weeks.
• Thromboembolism (blood clots)
Blood clots in the leg veins rarely happens after knee replacement. Clinically important thrombosis occurs in around 2% of the cases. Blood clots can form in the deep veins of the legs or pelvis after surgery. Blood thinners such as low-molecular-weight heparin, and aspirin can help prevent this problem. Newer blood thinners, such as apixaban (Eliquis) and rivaroxaban (Xarelto), may also be prescribed by depending upon your needs.
• Injury to nerve or vessels
Although it rarely happens, nerves or blood vessels may be injured or stretched during the procedure. Some small nerv branches to the skin will be inadvertedly cut and this may create an area of numbness around the skin incision. This doesn’t cause any functional problem or discomfort to the patient.
• Persistent pain and/or knee stiffness
• Anaesthetic risks
• Need for further surgery
As explained already, some of the above mentioned adverse events may require further interventions for their treatment.